Fertility Burnout and Relationships: Why IVF Tests Even the Strongest Partnerships
By Margaret Cali, Fertility & Mindset Coach
Fertility challenges do not happen in isolation.
They happen inside relationships.
Inside shared hopes.
Inside conversations that slowly become harder to have.
Many couples enter fertility treatment believing that love and commitment will be enough to carry them through.
Often, they are surprised by how much strain IVF places on even the strongest partnerships.
This does not mean the relationship is failing.
It means the pressure is real.
How Fertility Burnout Shows Up in Relationships
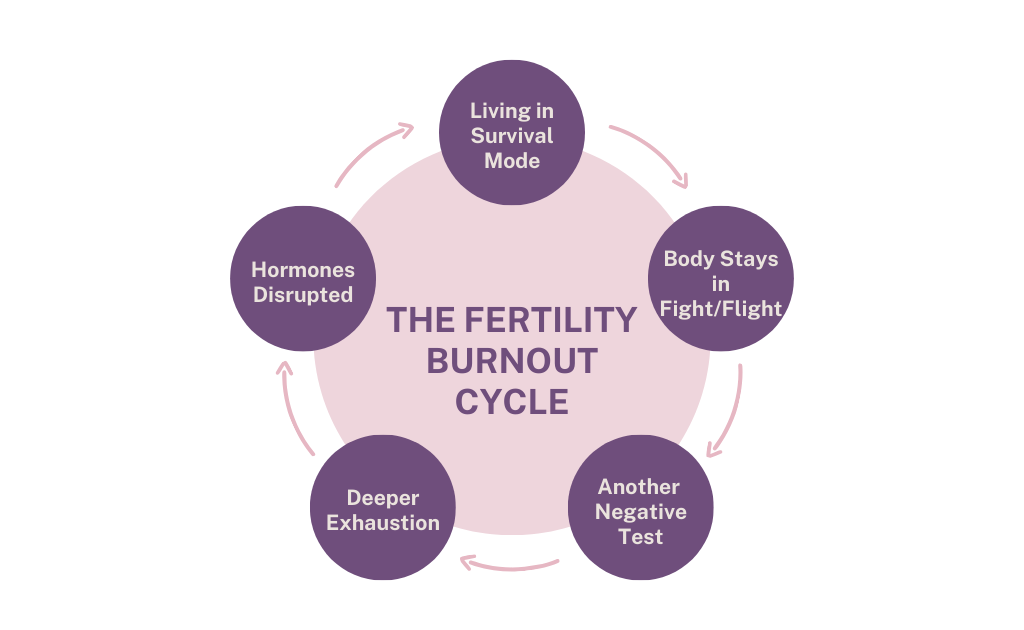
Fertility burnout does not only affect the individual going through treatment.
It seeps into:
-
Communication
-
Intimacy
-
Emotional availability
-
How partners interpret each other’s responses
Common experiences include:
-
Feeling alone even with a supportive partner
-
One partner wanting to talk, the other shutting down
-
Scheduled intimacy replacing connection
-
Avoiding difficult conversations to “keep the peace”
-
Carrying grief privately to protect the other
Many couples are still showing up.
They are still committed.
But something feels heavier than it used to.
Support Is Not the Same as Alignment
One of the most painful experiences women describe is this:
“My partner is supportive, but I still feel alone.”
Support often looks like:
-
Attending appointments
-
Saying the right things
-
Wanting to fix the problem
-
Staying optimistic
But alignment requires something different.
Alignment means:
-
Shared understanding of emotional load
-
Language for fear, grief, and uncertainty
-
Agreement on how to handle outcomes
-
Permission for both partners to struggle differently
Without this, couples can unintentionally drift apart while trying to protect each other.
The Invisible Load Many Women Carry
In fertility treatment, women often carry an invisible emotional and mental load.
This may include:
-
Tracking cycles and medications
-
Managing appointments and results
-
Absorbing family questions
-
Holding hope and disappointment simultaneously
-
Regulating everyone else’s emotions while suppressing their own
Partners carry weight too.
Often silently.
But when the load is uneven or unspoken, resentment and misunderstanding can grow.
Not because of a lack of love.
But because of a lack of shared language.
Why IVF Amplifies Relationship Patterns
IVF does not create relationship problems.
It amplifies what already exists.
Patterns around communication, conflict, avoidance, or emotional expression become more visible under pressure.
Couples may notice:
-
Old coping strategies no longer work
-
Small misunderstandings feel bigger
-
Emotional shutdown in one partner triggers fear in the other
-
Both partners feel misunderstood in different ways
This is not a sign to panic.
It is a sign to slow down.
What Helps Couples Stay Connected During Fertility Treatment
Connection during fertility challenges does not come from trying harder.
It comes from clarity.
Helpful shifts often include:
-
Naming what each partner is actually feeling
-
Asking for specific support rather than assuming
-
Agreeing on boundaries with family and friends
-
Remembering that you are on the same side
-
Making space for grief and hope to coexist
Sometimes, the most protective thing a couple can do is learn how to talk about the hard parts without trying to solve them immediately.
Preparing the Relationship, Not Just the Body
Most clinics prepare the body for IVF.
Very few prepare the relationship.
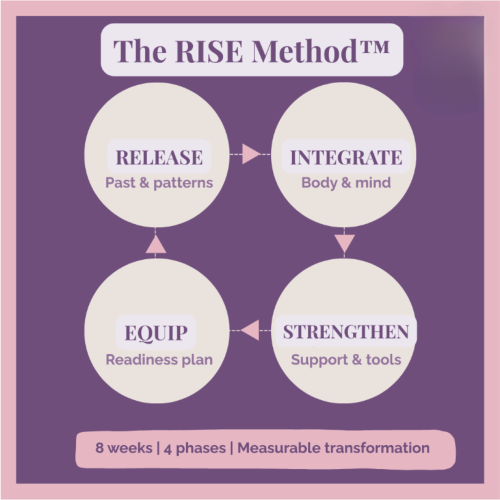
Emotional readiness before treatment includes:
-
Communication tools
-
Nervous system regulation
-
Shared expectations
-
Space to process fear together
-
Permission to not be “strong” all the time
When couples feel emotionally prepared, IVF still feels challenging — but less isolating.
You Are Not Doing This Wrong
If your relationship feels strained, distant, or fragile during fertility treatment, it does not mean you are failing.
It means you are navigating one of the most stressful experiences a couple can face.
With support, language, and intention, many couples find their way back to connection — sometimes with more depth and honesty than before.
Where to Go From Here
If this post resonated, you may also find these helpful:
-
The Truth About Fertility Burnout — And Why Emotional Readiness Matters More Than You Think
-
Emotional Shutdown During Fertility: When “I’m Fine” Is a Survival Response